“Terrible Culture of Blame"
When did:- “Don't worry, we will absolutely keep you safe" ¹
Change to:- “Don't worry, if we accidentally kill you, we will definitely learn lessons from it".
In March 2016 then UK Health Secretary Jeremy Hunt said “It is a scandal that every week there are potentially 150 avoidable deaths in our hospitals and it is up to us all to make the need for whistleblowing and secrecy a thing of the past as we reform the NHS and its values and move from blaming to learning”.
Then in June 2022 Mr Hunt spoke of the “Terrible NHS Blame Culture”.
Wait a minute. I appreciate that health professionals are human, but professionals have to understand that they are accountable for their life and death mistakes. If not, how can anyone have confidence and trust in the care they provide. Do we really see patients’ lives and wellbeing as potential collateral damage, as staff “learn", and then move on to the next case. If there exists a “Terrible Culture of Blame” in the NHS, this suggests that too many things happen for which people should rightly be blamed.
You may feel “Collateral damage" is too strong, too controversial, too emotive a term to use.
Perhaps. Until we remember the untested Covid-infected patients that were offloaded by NHS hospitals to care homes supposedly sheltered by Health Secretary Matt Hancock's “Protective Ring of Steel”, and the number of elderly care home residents who, as a consequence, contracted the virus and died in isolation from their families and friends.
The plain fact is, the NHS juggernaut is pathologically incapable of learning from previous scandals.²
“Good Deaths”
Not the 150 a week avoidable ones, part of what follows was deliberate.
A respected health care influencer blocked me on Twitter because I described how between 2003 and 2014 certain English hospitals had been drugging elderly patients then starving them to death. It happened. It was called “The Liverpool Care Pathway” (LCP), and notwithstanding the name, the practice was not confined to the City of Liverpool. In less complimentary circles, LCP earned the then Health Secretary the nickname “Midazolam Matt”. A hospital doctor commentating on Twitter claimed there was no abuse of Midazolam. So I asked him whether he found the LCP’s “Good Deaths” ethically and morally acceptable. He dodged the question. As far as I am aware, no one involved has ever been held accountable.
Contrast Liverpool Care Pathway (LCP) with the Gosport War Memorial Hospital scandal. While the allegations forming the Gosport scandal pre-date LCP, there are distinct parallels between the two. It is alleged that between 1989 and 2000, 456 elderly patients had their lives cut short through the unlawful administration of high doses of opioids³. There was a lamentable failure by Hampshire Police to properly investigate, amid allegations of cover-up, corruption and scapegoating.
The Gosport investigation was taken over by Kent and Essex Serious Crime Directorate in April 2019 as Operation Magenta. After assessing over 750 medical records and 1150 witness statements from family members, 19 suspects have been identified and are being interviewed under caution.
These are major scandals we know about.² That they have come to public attention is due in large part to the unflinching tenacity of family and friends of the deceased, in exposing the truth.
Whilst human judgement is fallible, and professionals can make mistakes, on rare occasions decisions are made that are perverse or downright malevolent. What I find absolutely unforgivable are NHS denials and “cover-ups”, depriving family and friends of the true facts. No one really knows how many more scandals may have been buried by aggressive anti-whistleblowing policies.
As if to underscore these concerns, the latest in a string of NHS whistle blower sackings emerged at Brighton’s Royal Sussex County Hospital. Two renowned surgeons lost their jobs after raising concerns about malpractice and patient safety in neurosurgery and general surgery. Sussex Police are investigating 19 deaths and 23 cases of serious patient harm alleged to have occurred between 2015 and 2020. For those families, now alerted to the probability that their loved ones did not receive the care they deserved, this must be a truly awful time.
This continuing “cover up” culture in the NHS undermines any foundation on which to build confidence and trust.
I’m 69 and unpaid carer for 2 vulnerable ladies. I do not want a hospital-acquired infection. And I do not want to be drugged to the eyeballs on God-Forsaken ward, waiting to die a miserable, lonely death, with the true facts withheld from my family.
“Ah… the NHS will say, that’s all in the past.” I’m not convinced.
Without Trust, the canula they put in your arm is scary. You have no clue, no control, no trust, as to what the NHS might put into your body.
“Complications"
We sometimes hear of an unfortunate patient who entered hospital for a supposedly routine procedure, and then died or suffered harm from “complications”. Which makes me wonder about “complications”. What is a “complication”?
Poor aseptic technique?
Hospital-acquired infection?
Ineffective antibiotics?
An event or underlying condition that the doctors failed to identify or anticipate?
Cost cutting exercise?
Or perhaps, just a plain “cock-up”
Or could this be a euphemism for “cover up”? Surely not!
Disgruntled Staff
An already desperate situation has been exacerbated because overworked, underpaid, disgruntled hospital staff consider they have been left with no option but to take industrial action. The implied government line that clinicians’ love of their vocation should trump their need for a decent level of pay, and safe working conditions for them and for their patients, just doesn’t wash anymore.
Primary Care
I see “our” GP once in a blue moon. He doesn’t like me, and I don’t trust him. On one rare encounter, he didn’t notice the nosebleed I was having, sitting right in front of him. This is the same guy who banned me from carers’ health checks.
So, which would you prefer, a newly qualified, fresh faced doctor well versed in the very latest academic research and diagnostic techniques, who understands the exponentially growing relevance of AI and other technologies… Or a disillusioned, albeit experienced, dyed-in-the-wool practitioner marking time to their early retirement and their pension. (Rhetorical)
My first instinct was that numbers of the former would be declining, with those of the latter increasing, as more overworked GPs near retirement. I was wrong. The numbers of both groups are declining relative to the population they serve. It is estimated nearly half of GPs want to retire before they reach 60.
“…the NHS is in the midst of a chronic workforce crisis, driven by years of insufficient investment in training new staff, inadequate workforce planning, and lack of government accountability…”⁴
“The NHS has lost the equivalent of 2,133 full-time fully qualified GPs since 2015.”⁵
“Whilst the GP workforce is declining, the number patients continues to rise. In April 2023, a record-high of over 62.4 million patients were registered in England. As a result, the average number of patients each full-time equivalent GP is responsible for continues to rise, and now stands at 2,292. This is an increase of 355 patients per GP, or 18.3%, since September 2015, demonstrating the ever-mounting workload in general practice.”⁵
Current health secretary Steve Barclay recently announced £240 million funding to improve GP services through improved use of technology and using receptionists as expert “Care Navigators”. Whilst any funding increase is to be welcomed, this relates to availability of appointments rather than provision of more doctors - little more than a sticking plaster.
Primary care needs more GPs. It can take up to 10 years to train a new GP , exposing a woeful lack of forward work force planning:-
A medical degree - usually takes 5 years
Doctor foundation training - usually a further 2 years
GP training under supervision - usually 18 months in a hospital then 18 months in a GP practice.
Then Health Secretary Jeremy Hunt said:- “We’re training more doctors than ever before”. Welcome news, you’d think, until you realise that the log jam is in insufficient post graduate foundation and specialist training places.
Can it be saved
Whilst I intended this post be about trust (or not) in the NHS, it would have been remiss not to summarise the roles of workforce planning and funding. Funding stream details are complex, particularly in relation to GP practices, and therefore beyond the scope of this article.
Nye Bevan’s 1946-8 model has become increasingly difficult to resource and sustain. Reduced availability of key services, delays, longer waiting times, shortage of doctors and nurses, and decaying estate were already evident before the Covid pandemic.
The British Medical Association (BMA), the trade union and professional body for doctors in the UK said:- “Although NHS spending has increased, it has not increased enough to keep up with demand. There has not been enough investment in infrastructure, which means there are not enough beds in hospitals and some estates are unsafe. Staff have also had to put up with sub-inflationary pay rises since 2008, leaving them feeling undervalued and burnt out.”⁵
Several critical strictures have been at play:-
extortionate PFI contracts with the private sector, used to finance over 100 new buildings from 1992
more recently, dodgy PPE contracts
waste
expensive clinical errors
an increasingly litigious society
increasing demand
increasing costs of treatments including drug prices
bed blocking - directly attributable to inadequate social care provision
aging population, often with multiple morbidities and more complex chronic health needs
On one hand there are widely held suspicions that during the 13 years they have been in government, the Conservatives have deliberately run down the NHS in order to open opportunities for privatisation. It is true that some additional funding was allocated, but it was nowhere near enough.
“The increases in NHS spending agreed by the government were insufficient to deal with the costs of rising demand and deficits that had built up after five years of constraints. Winter pressures from 2014/15 onwards made the effects starkly visible as patients encountered overcrowded A&E departments, long waits on trolleys for hospital beds, and cancelled operations.”⁶
On the other hand Labour in opposition are unlikely countenance substantial increases in personal and corporate taxation to adequately fund the NHS, because to do so would be electoral suicide. And proposed one off “windfall taxes” will not open up consistent revenue streams.
With no clear political will on either side to develop an imaginative, radical funding policy, the NHS will continue to run on an financial knife edge. The possibility of eventual implosion cannot be ruled out.
Artificial Intelligence AI
I may be pilloried for this suggestion.
AI, Artificial Intelligence, coupled with state of art computer vision, scanning and monitoring will assist in saving the NHS, especially for primary care. AI can access millions of instances of diagnostics data and anonymised disease histories in seconds. Chatbots such as GPT4 and Bing Chat do not have inherent “intelligent” power to reason, but their ability to process massive stored data and language provides an extremely convincing impression that they are able to do so, holding (for example) their end of high level debates with human philosopher
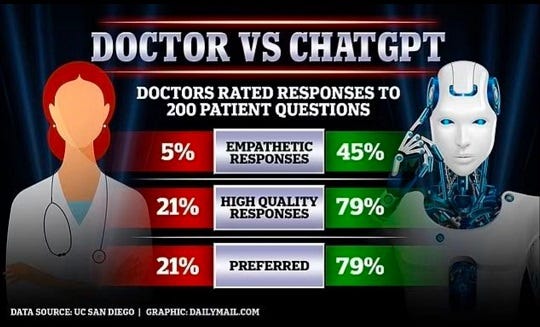
about the Stoics and Stoicism. These abilities can be applied to clinical imaging, monitoring, note taking, and most significantly of all, diagnostic consultation and routine prescribing.This is just one study, but it echoes anecdotal findings elsewhere. In clinical settings interacting with humans, ChatBots can perform impressively on ratings for empathy, accuracy, and overall user preference.
We know also that AI Chatbots have a tendency to “hallucinate” (tell lies), when they run out of answers. Nonetheless, on balance, I think would trust a healthcare AI Chatbot just that little bit more than I would trust an overworked, stressed out, fallible human GP.
Conclusion
So, can I trust the NHS?
Right now? No.
Frustratingly, I cannot find the post where where I read this…
We should stop using the term “patient” because "patient” implies a powerless submissive recipient. They are Clients, entitled to a high quality service. What is required is a two way “Client - Provider" relationship.
1. Unnamed front line A&E doctor amid Covid crisis
2. I’ve taken some of the more well known historical scandals as read:- Thalidomide, Primodos, blood products, vaginal mesh, Mid Staffordshire…
3. Gosport Independent Panel Report.
4. BMA bma.org.uk 25/5/2023
5. BMA analysis of NHS General Practice Workforce Data
6. The King’s Fund: Rise and Decline of the NHS in England 2000-20
You might like one or more of my previous posts…
Covert Carer
Why…? My first COPING WITH CARING Substack post outlined that I’m unpaid care giver for two vulnerable ladies, my mother aged 99 and my wife aged 67. Care giving creates a new, unexpected, hectic chapter in the carer’s life. Familiar home routines are scrambled, Sky Sports is cancelled, and “want-to-do” lists are consigned to the waste bin.
Nearly Talking of Robots
Whilst I don’t have a great deal of time to devote to them nowadays my robot and train projects continue (slowly) as my occasional escape from care giving. Last night, I became so frustrated with my inability include a short video clip in a reply to a note (most likely operator error), that I decided to create this new post.
The Summerhouse
We were startled by the bang. A toughened pane in a rotting frame just shattered, scattering a thousand glistening diamonds to the ground. “Help me!” it screamed. “Please don’t neglect me into decay and nothingness…” I’m so glad we didn’t. I made it better. Roof re-membraned. Wood re-coated. Oversized doors from eBay cut to fit. Windows of clear…
Helpful Things
There are simple low tech items that can make a big difference when you are a carer. Here are a few I use. This whistle-stop tour is not intended in any way as promotional… Plug-in Night Light A plug-shaped light which fits in a mains socket to light automatically when darkness falls. The gentle glow in bedroom and hall provides a safer, comforting en…










The state of public healthcare in the UK is terrifying indeed - but I believe a massive part of our problem is not so much that politicians are afraid to raise the taxes required to provide more funding, but that they're so incoherent in terms of their own ideologies that they can't argue one way or another about whether the NHS is desirable in principle or in practice. They *could* argue for higher taxes here, or reduced spending there, or investment here to stimulate growth there, on the basis that the NHS, as a point of principle, is worthwhile and that our country deserves a viable, well-run public health service - but they won't. From top to bottom, all of our major parties are taking money and freebies from private health interests, and once their stint in parliament is ended, plenty of MPs will trot off to provide consultancy services to one or more of them.
It's one thing for the NHS to die because of lack of funding - but it's quite another for it to die because our own politicians simply won't argue for it other than it being 'free at the point of use' - which is no good to anybody if the service is terrible!
As it stands I can't see the NHS lasting to my retirement age - but I'd bet an arm and a leg that no matter what kind of dire situation the economy may be in at any given time, there will *always* be a way to fund whatever it is our politicians actually do want, which most of the time seems to be war and bungs for their mates!
The arguments you present here - highlighting the scandals, the problems with recruitment etc - we need to hear these things coming from the mouths of politicians if we are ever to save the NHS. The money exists, but the will doesn't, unfortunately!
hey where you vanished.....? ((((